3.5hrs saved per 50 claims processed
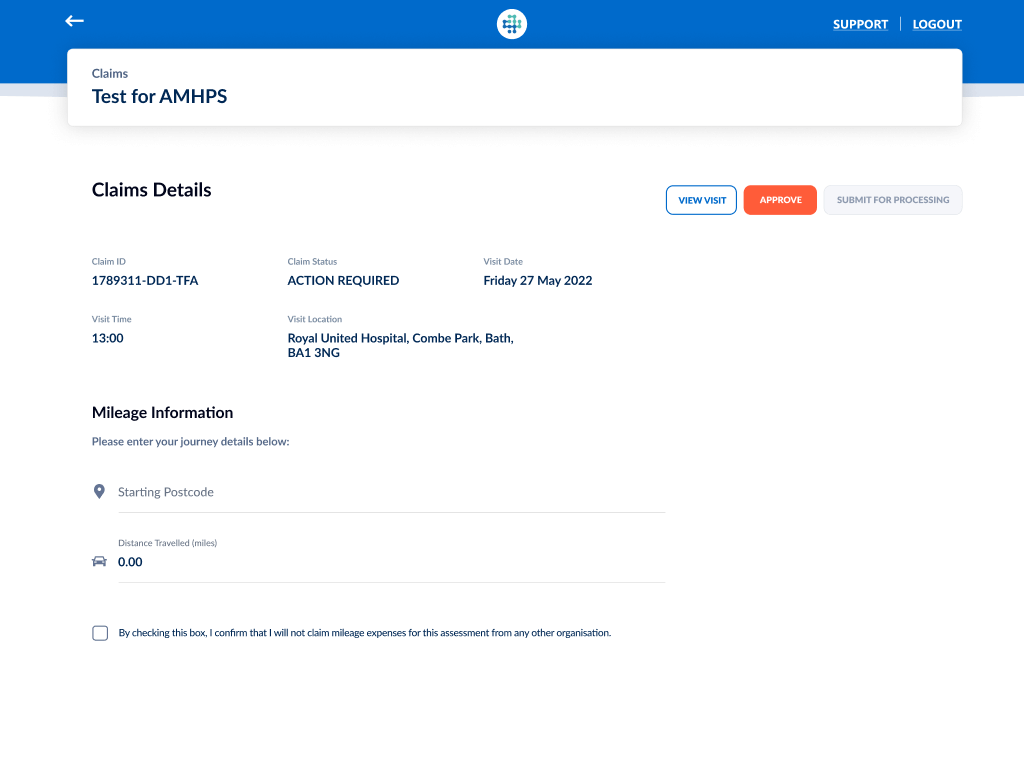
S12 Electronic Claim Forms
S12 Solutions provides an electronic means of creating, submitting and processing section 12 (s.12) doctors’ claims for MHA assessments.
GDPR compliant
Patient information is sent and stored securely using a standardised, GDPR compliant process
Larger doctor network
Doctors are more likely to take on s.12 work, and have the confidence to work beyond regional boundaries, increasing the likelihood of timely MHA assessments
Increased productivity
Processors have more time to focus on other tasks
Improved budget management
Budget issues associated with bulk submissions are removed
Environmental benefits
Digitising the process supports ‘Delivering a net zero NHS’ ambitions
Standardised, GDPR compliant claim form process for Section 12 doctors
Case for change
In some cases, Section 12 doctors can claim a fee for attending MHA assessments, but the manual process used to make the claim often causes problems. Paper forms containing comprehensive sensitive patient information were shared using non-secure methods and handled by multiple people. Issues such as regional process variance, incomplete or illegible information, and bulk submissions, meant paper forms could take a long time to process or were not processed at all. Doctors did not always know where to send claims or how to resolve slow or missing payments.
System consequences
In many cases, these problems discouraged doctors from taking on additional s.12 work, reducing the network of doctors available to approved mental health professionals (AMHPs); relying on a small pool of known doctors made it harder to organise timely assessments and assemble s.12 doctors with the best-fit experience for the person being assessed, in line with the MHA Code of Practice.
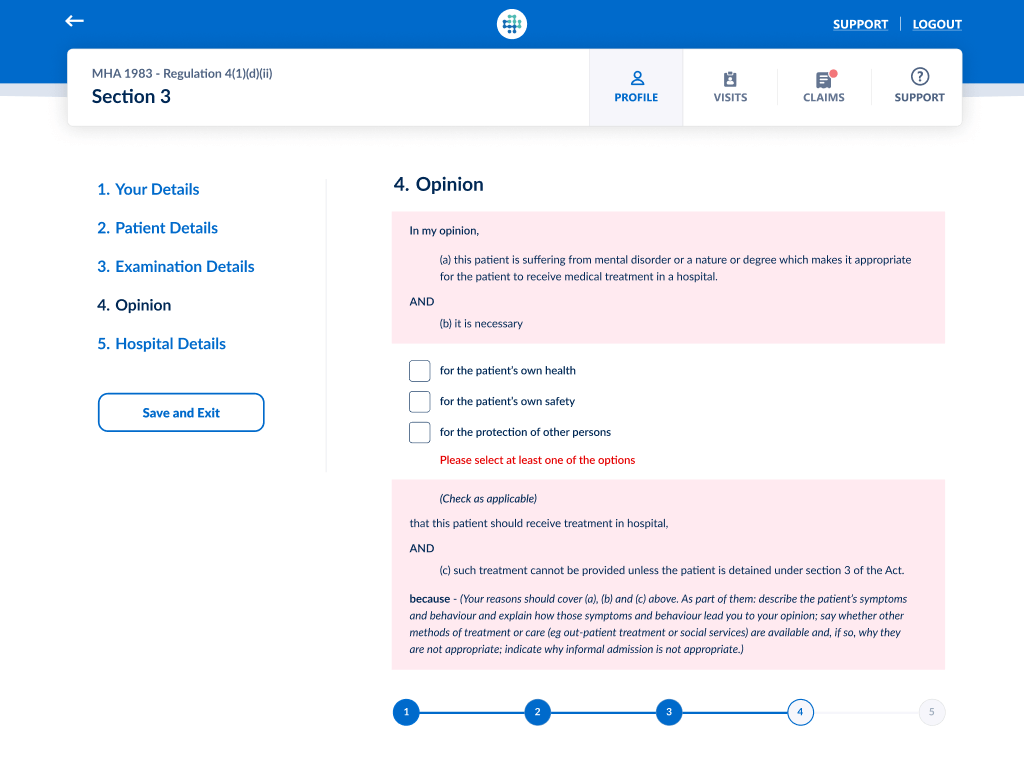
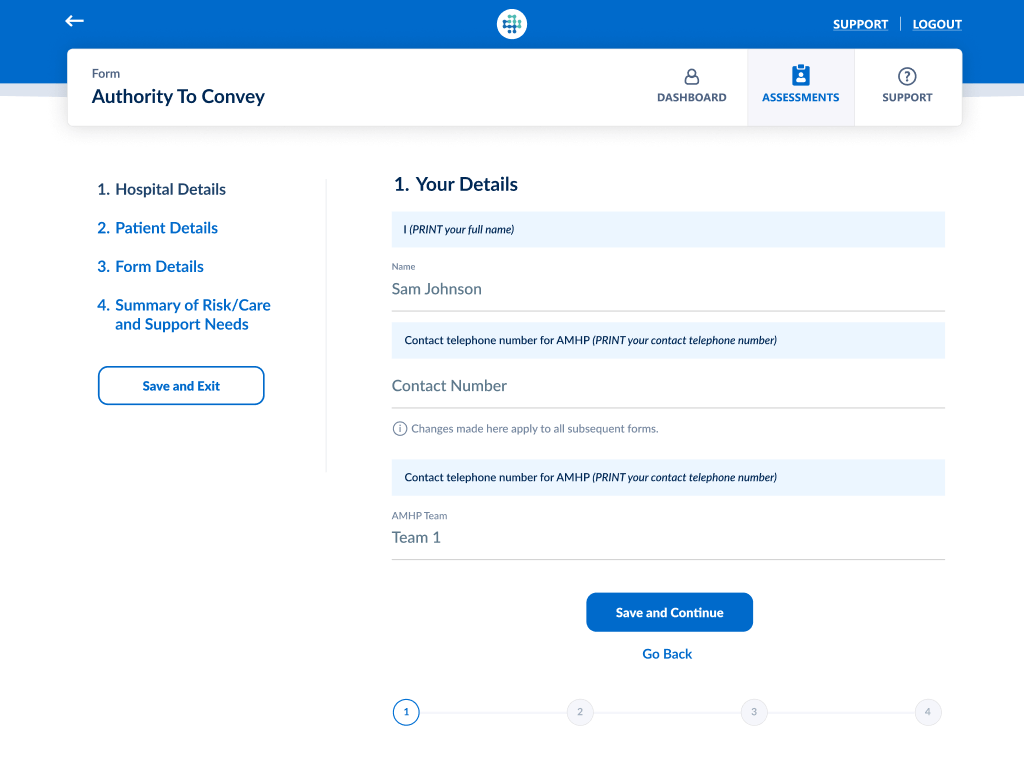
A secure, standardised process
S12 Solutions addresses these issues by enabling doctors to submit electronic claims, directly to the paying organisation, and follow the progress of their claims in their Claims Dashboard. GDPR compliant information is transferred securely, and processing and budget management are more efficient for claims and finance teams.
What makes it different?
The only solution to all S12 Doctors to submit electronic claims
AMHPs create claims and answer up to three questions in line with NHS England’s Who Pays guidance, to determine which organisation is responsible for paying the claim
Doctors complete their claims and submit to the paying organisation(s) for processing
Doctors can see which organisation(s) are processing and paying their claims
Processors review and process claims
Doctors can also see whether their claims are under review, approved, rejected or paid
92% of Drs paid faster