blog
-Demand & Capacity
Discharge Audits
Discharge Management
Patient Flow
Planned Care
Urgent Care
How identifying patients ready for discharge is optimising patient flow
We’ve interviewed Claire Basden, Clinical Account Manager at VitalHub UK for MCAP, who explains how identifying patients ready for discharge is helping trusts free up beds and optimise patient flow.
Claire began working with MCAP in 2014, having previously worked in several healthcare settings across primary and secondary care and the community. Claire is a registered practitioner (RGN) with 20 years of experience of working within the NHS, including hands-on care delivery and management experience. As a community nursing service manager, she has extensive experience in delivering high-quality clinical care, and as a Pathway Redesign Lead, she has experience in leading on the redesign of services and pathways.
In her role as Clinical Account Manager for VitalHub UK, Claire supports the implementation of Clinical Utilisation Reviews (CUR) using the MCAP platform, across several NHS trusts in the UK, Australia, and Qatar. MCAP is used to identify the challenges in patient flow as well as helping healthcare organisations make informed decisions around future commissioning intentions.
Claire, in what context has MCAP been developed to support NHS trusts?
“Across the NHS, delays to discharging patients from hospital when they are fit to leave has become a significant issue. It’s a problem that has been highlighted regularly in recent conversations I’ve had with local authorities, social care and NHS providers – who are saying the most pressing issue they are facing is a lack of available beds for patients who need them – and the knock-on effect of extended and unnecessary time spent in hospital by people who are better placed recovering at home, or in residential care.”
“The extra focus on needing to free-up beds to help manage the huge backlog caused by the pandemic is also a pressure point, and it’s well documented that longer hospital stays can lead to worse outcomes for patients – particularly around deconditioning.”
“Recent NHS data outlines the impact deconditioning because of delayed transfers can have on patients, including that, for older patients, it contributes to delayed discharge for more than 45%, and that half of patients experience functional decline between admission and discharge.”
“But what if there was a way trusts could empower hospital teams to maintain patient flow in and out of hospital more efficiently by using data to safely identify patients in hospital who are clinically suitable for discharge, or even non-admission? That’s where MCAP is making a difference.”
How does MCAP work and what digital technology does it use?
“In a nutshell, MCAP is a real-time clinical decision support tool that identifies patients who are clinically suitable for discharge or non-admission.”
“Rather than calculating expected discharge based on an average or general care pathway, MCAP is based on an objective analysis of a patient’s individual care service requirements – identifying patients that can be moved to alternative pathways, with the goal of enabling treatment of the patient as close to home as possible, where possible.”
“Because the MCAP solution is integrated with hospital systems, this data is available to all levels of management within any Integrated Care System, which avoids the duplication or silo of patient information.”
But could the use of MCAP be viewed as denying patients the care they need?
“MCAP doesn’t exist to deny care, but to place patients at the correct level of care given their individual needs, while supporting trusts and hospitals to optimise their flow of patients and – ultimately – make more beds available for patients awaiting treatment.”
“Typical results in over 175 UK hospitals identify that around 25% of admissions, and 50% of continuing care days, could be avoided or delivered in an alternative way – with typical savings of at least 60% on those care days.”
“Crucially, because it is based on services needed to control and reduce the clinical risk of an individual patient, MCAP automatically accommodates co-morbid and co-occurring conditions. It doesn’t exist to challenge or change the physician’s diagnosis or treatment plan, but instead optimises how the treatment plan is delivered.”
How does MCAP help future-proof care delivery?
”If a trust can quickly analyse and understand demand and capacity in the secondary care system based on the current acuity mix of patients, future care planning becomes significantly more informed. For example, teams can understand the number of admissions that can be deferred to avoid admission caps or winter overload, the amount of potentially avoidable continuing days of care to shorten length of stay, and the levels of care that are required to achieve both.
“At ICB / CCG level, MCAP’s reason code analysis can be used to support and inform operational and strategic planning while also providing additional evidence for a future business case and service reforms, and can help to shape reporting processes by providing information to develop trigger levels, such as an acceptable number of patients awaiting service on a given day.”
“The technology also supports initiatives such as The National Health and Social Care Discharge Taskforce, helping ICBs/CCGs to evidence of robust discharge processes through gathered data including avoidable length of stay, and the number of beds occupied by patients clinically ready to be discharged to more appropriate care settings.”
“With the recent impact assessment of the Health and Care Act by the Department of Health and Social Care highlighting that wider use of Discharge to Assess (D2A) could free up as many as 6,000 hospital beds and save the NHS £7bn by 2031, it is widely agreed that patients should be supported to return to their home for assessment whenever and wherever possible.
“By determining the capacity needs across a system and directly supporting hospitals to implement a discharge to assess model where going home is the default pathway, MCAP is helping make this a reality.”
NEXT STEPS | Book an MCAP Snapshot Discharge Audit
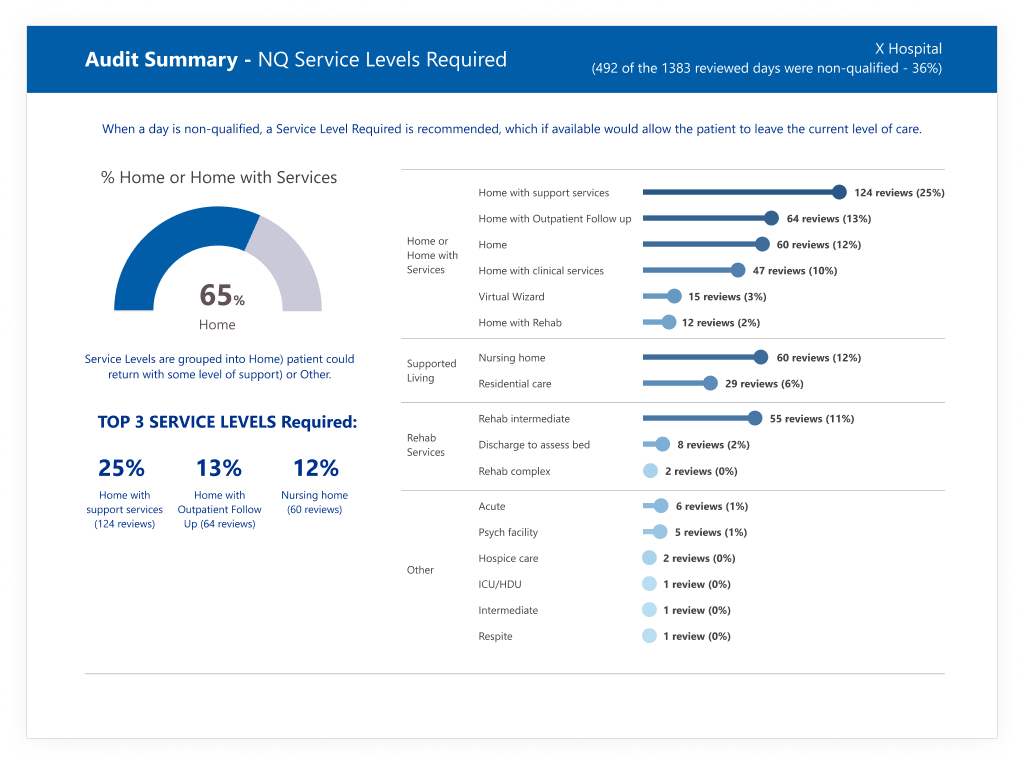
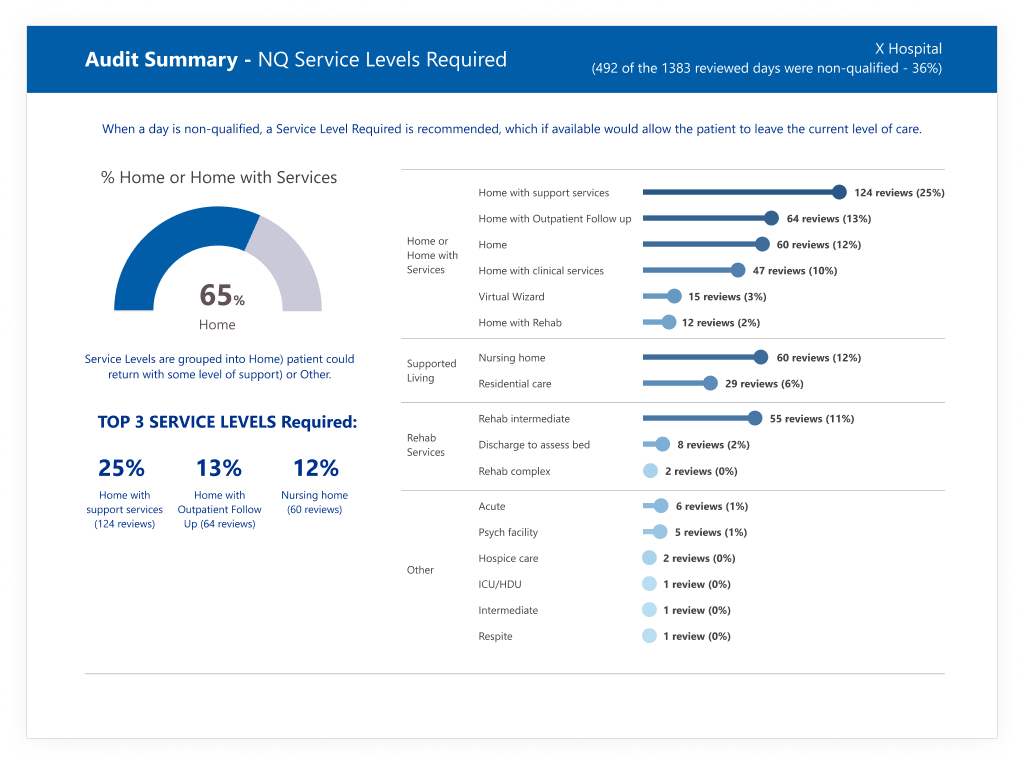
Delivered by our team of trained nurses, an MCAP Snapshot Discharge Audit identifies patients who are non-qualified to reside in a hospital bed and defines the most appropriate level of care for the patient outside of hospital, given their clinical need.
The audit is powered by our MCAP clinical decision support solution and conducts and analysis of 100 acute beds to produce an analysis of:
- Demand capacity
- Number of deferrable admissions
- Level of potentially avoidable continuing care days
- Internal and external blockages preventing reductions is admissions / length of stay
Some of the benefits of our Discharge audit include:
MCAP has been used to audit over 175 hospitals and has been able to identify twice the number of patients that can move to alternative pathways and 50% of continuing care days that could be avoided.
Allows informed decisions about how best to focus resources to generate the greatest impact on safely flowing patients and freeing beds.
Analysis of the demand and capacity, internal & external blocks and shorten Length of Stay.
To book your Snapshot Discharge Audit, contact the team on: mcap@vitalhub.uk