A reduction in delays and an annual saving of £324,000 per annum
MCAP
MCAP is a clinical utilisation review system that supports healthcare organisations to tackle patient flow, delayed transfers of care and stranded patients, by identifying opportunities to reduce Length of Stay
Why MCAP?
Identify the right level of care for patients
Enable clinicians to quickly establish if the patient is receiving care at the most appropriate level
Identify patients fit for discharge to alternative pathways
Support clinicians to identify patients fit for discharge to alternative pathways more appropriate for their individual care needs
Reduce average Length of Stay
Effectively manage the movement of patients and reduce delayed transfers of care, by identifying opportunities to limit unnecessary episodes of extended length of stay
Reduce departmental delays
Utilise data to support service redesigns to reduce delays and improve operational efficiency
Identify trends causing bottlenecks
Provides insight into the principal reasons for continued stays and subsequent delays.
Maximise efficiency of resources
Increases utilisation of clinical space, while also promoting faster patient rehabilitation through the avoidance of deconditioning.
When the MCAP challenge criteria is integrated into a patient flow module, it will identify TWICE the number of patients that are able to move to alternative care pathways than previous Medically or Therapy Fit For Discharge (MFFD or TFFD) processes.

Identify the right level of care for patients
It is well documented that longer stays in hospital can lead to worse health outcomes for patients due to deconditioning. Ensuring patients are in the right place, at the right time, based on their clinical need, is critical to avoid overcrowding and to reserve hospital beds for those who need them most. The MCAP clinical utilisation review software supports frontline teams to identify the right level of care for their patients, and identify patients fit for discharge to alternative pathways more appropriate for their individual care needs. MCAP improves patient care by supporting hospitals to tackle delayed transfers of care, stranded patients, and achieve a reduction in Length of Stay. MCAP also Integrates into existing systems, avoiding double entry of data and creating a ‘Single Version of the Truth’ for the wider Integrated Care System (ICS).

Understand root causes of patient flow blockages
MCAP’s specific, evidence-based clinical criteria identify the underlying root causes of patient flow blockages, these can be used to understand exactly what systemic issues the hospital is facing. MCAP utilises internationally recognised clinical criteria that is applicable to a range of specialities, including medical, surgical and mental health. The data is collected at patient level and aggregated to give a strategic view across the hospital, Integrated Care System (ICS), region or nationally, providing an objective and standardised methodology to measure reasons to reside. Only one criterion needs to be met for an admission or continued stay to be considered medically necessary.
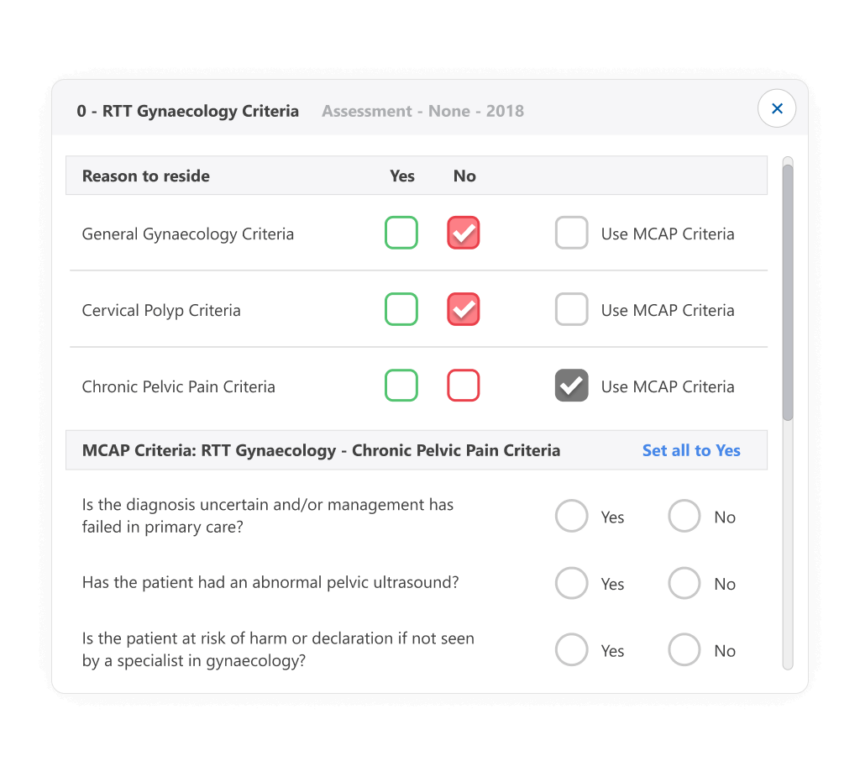
Utilise internationally recognised clinical criteria
The criteria within MCAP are considered best practice, evidence-based and have been adapted to embed local clinical practices and guidelines; such as the Discharge Guidance endorsed in the UK by the Royal Colleges of Medicine. The MCAP Criteria are comprehensive but easily understood by frontline staff. Data collected on MCAP is able to be utilised to automatically generate the national mandated discharge sitreps introduced in England in 2020, saving time for front-line staff and ensuring data is consistent and accurate.
What makes MCAP different?
The MCAP clinical utilisation review software supports frontline teams to identify the right level of care for their patients, and identify patients fit for discharge to alternative pathways more appropriate for their individual care needs.
MCAP utilises internationally recognised clinical criteria that is applicable to a range of specialities, including medical, surgical and mental health. The data is collected at patient level and aggregated to give a strategic view across trusts, providing an objective and standardised methodology to measure reasons to reside. Only one criterion needs to be met for an admission or continued stay to be considered medically necessary.
The criteria within MCAP are considered best practice, evidence-based and have been adapted to embed local clinical guidelines; such as the Discharge Guidance endorsed in the UK by the Royal Colleges of Medicine.
The MCAP Criteria are comprehensive but easily understood by frontline staff. Data collected on MCAP is able to be utilised to automatically generate the national mandated discharge sitreps introduced in England in 2020, saving time for front line staff and ensuring data is consistent and accurate.
Book a demoIdentify large numbers of patients that can be discharged
Identify barriers to the discharge planning process
Integrates into existing systems, avoiding double entry of data and creating a ‘Single Version of the Truth’
Utilises internationally recognised clinical criteria that are applicable to all specialities
Data collected is able to be utilised to automatically generate the nationally mandated discharge sitreps
Reduction in Length of Stay in target wards of 2.35 days
A 50% reduction in patients delayed due to pre-surgical admission
Reduction of patients delayed due to awaiting rehabilitation by 37%
100% increase in MFFD or TFFD patients