In 2022, almost 130,000 claims worth approximately nineteen million pounds were processed via the platform
Larger doctor network
Timely payment encourages more doctors to make themselves available for s.12 work, increasing the likelihood of timely MHA assessments
Improved productivity
Staff previously accountable for processing and paying claims have more time to focus on other tasks
Easier budget management
Processing claims regularly supports the accountable organisation’s real time cost management
Processes and pay section 12 (s.12) doctors’ claims every two weeks with an easy to manage online platform.
Case for change
The paper forms used by doctors to claim fees for attending MHA assessments took time to complete and required sensitive patient information to be transferred using non-secure methods. Processing paper forms was also time consuming for claims teams; processors had no easy way to retrieve missing information or identify duplicate submissions; claims sent in bulk, sometimes relating to assessments that took place in the previous financial year, caused problems for budget management.
System consequences
Consequently, payments were often delayed or doctors were not paid at all, dissuading doctors in some cases from participating in s.12 work beyond their contracted commitments. Relying on a small network of doctors made it harder for approved mental health professionals (AMHPs) to organise timely assessments, and assemble MHA assessment teams that were the best fit for the person being assessed, in line with the MHA Code of Practice.
Payments on Submission
In response to these problems, S12 Solutions codesigned a process with a mental health trust (trust) that enabled S12 Solutions to pay doctors’ claims, on the trust’s behalf, within two weeks of submission. The S12 Solutions team worked with the trust to introduce policies to support timely submission, and a communications plan to inform doctors about the changes. This process is now available nationwide.
What makes it different?
Using S12 Solutions to pay as well as process claims leads to improvements in productivity, compliance and timely Mental Health Act (MHA) assessment team organisation.
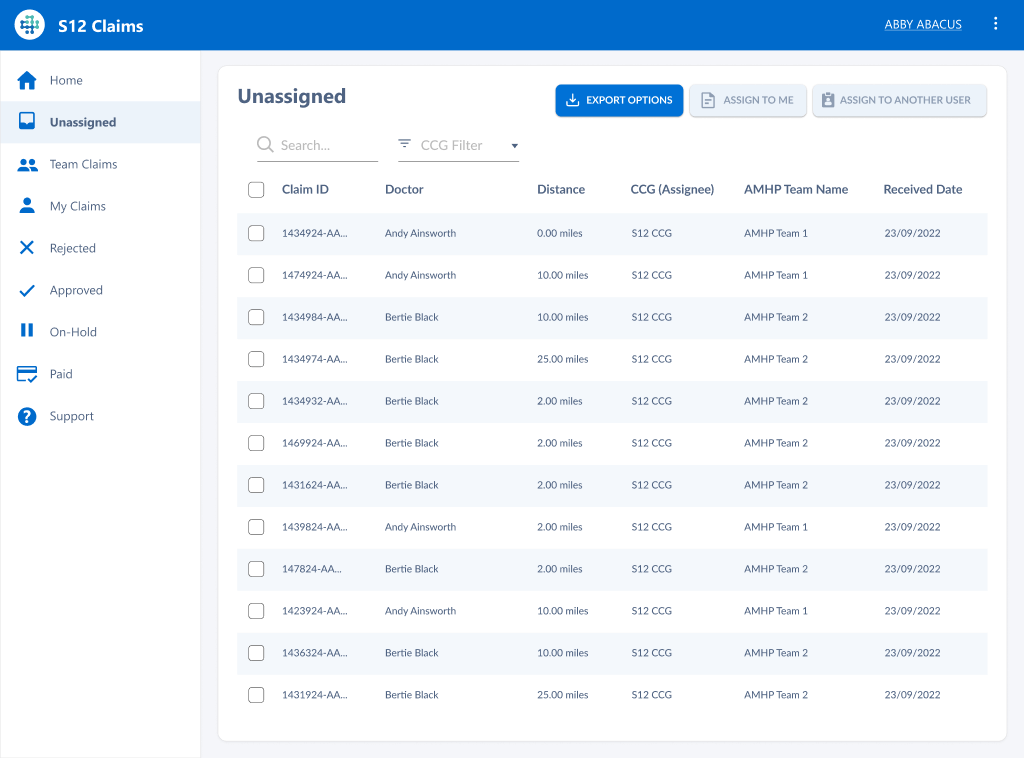
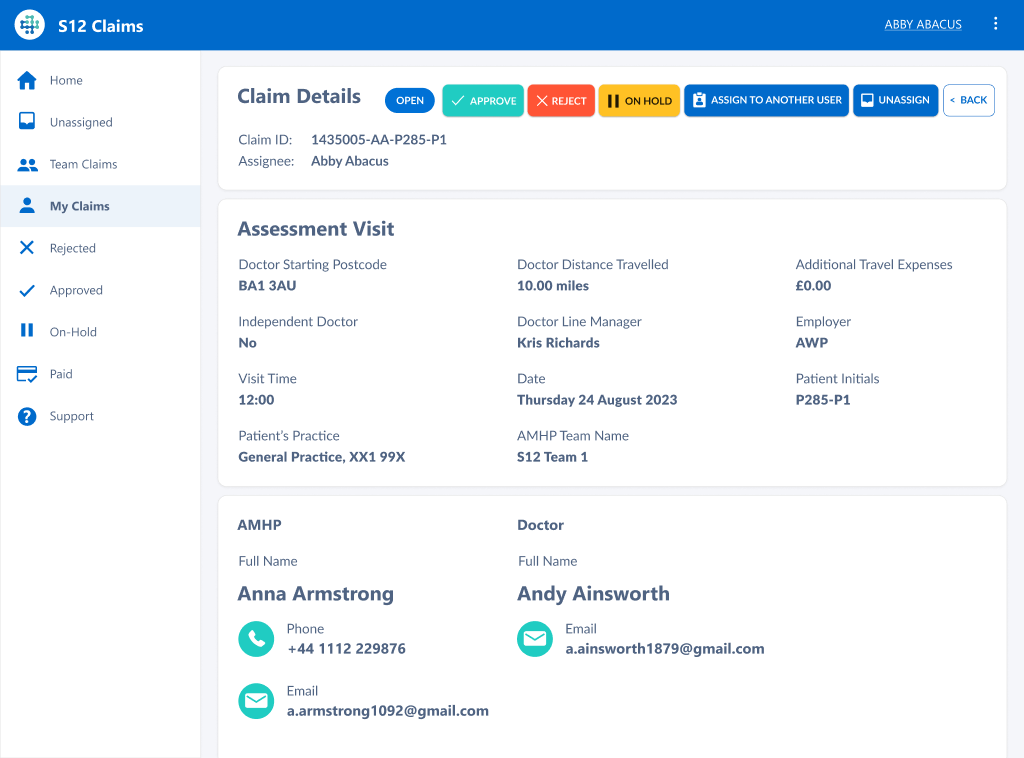
S12 doctors complete and submit their claims to S12 Solutions’ administrator via the platform
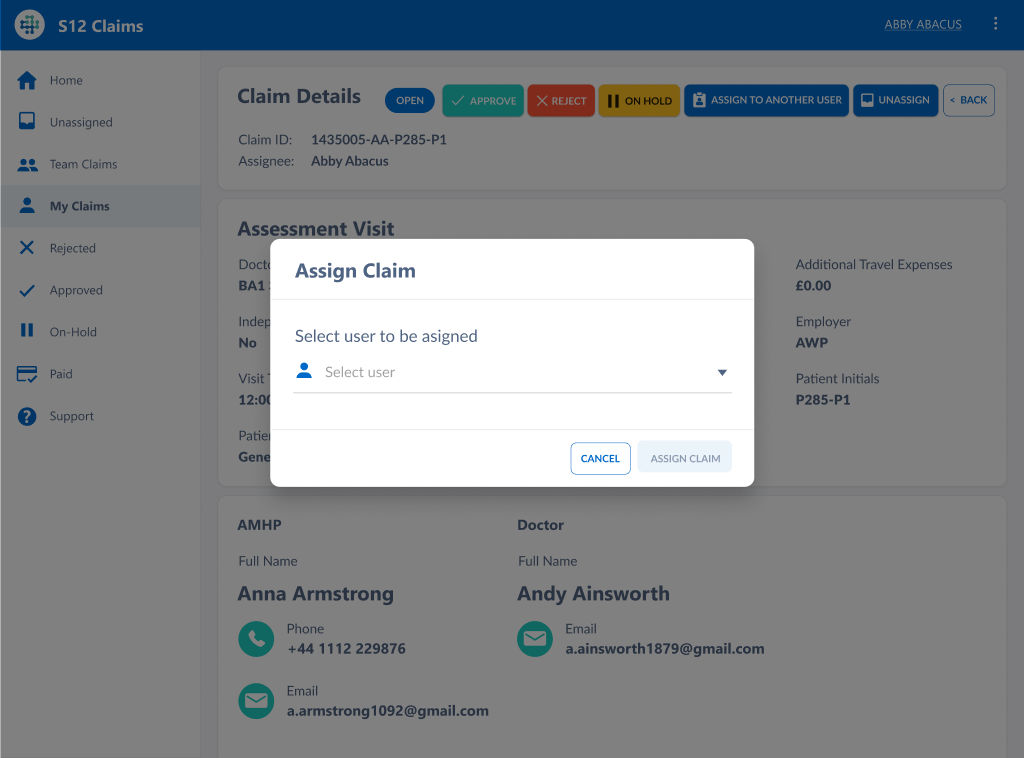
The administrator processes the claim according to the accountable organisation’s policies
Eligible claims are approved and ineligible claims are rejected
The administrator pays doctors’ approved claims
This process is completed every two weeks